
Medicaid Reimbursement
Medicaid Reimbursement
States with Remote Patient Monitoring Coverage
19 states have some form of coverage and reimbursement for RPM. Most States pay a flat rate per day ranging from $6 to $12 that covers all of the equipment, vendor fees for the software platform and the clinician time to run the monitoring program.
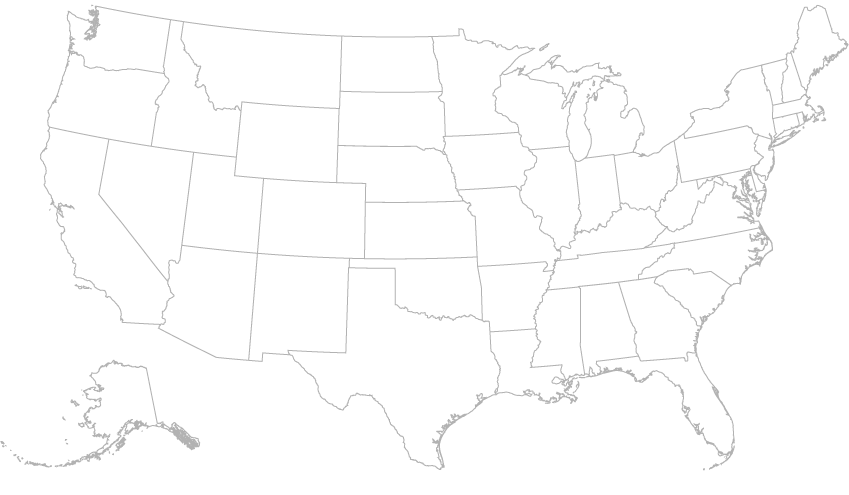
Learn more about each State and what specific Reimbursements they offer.
