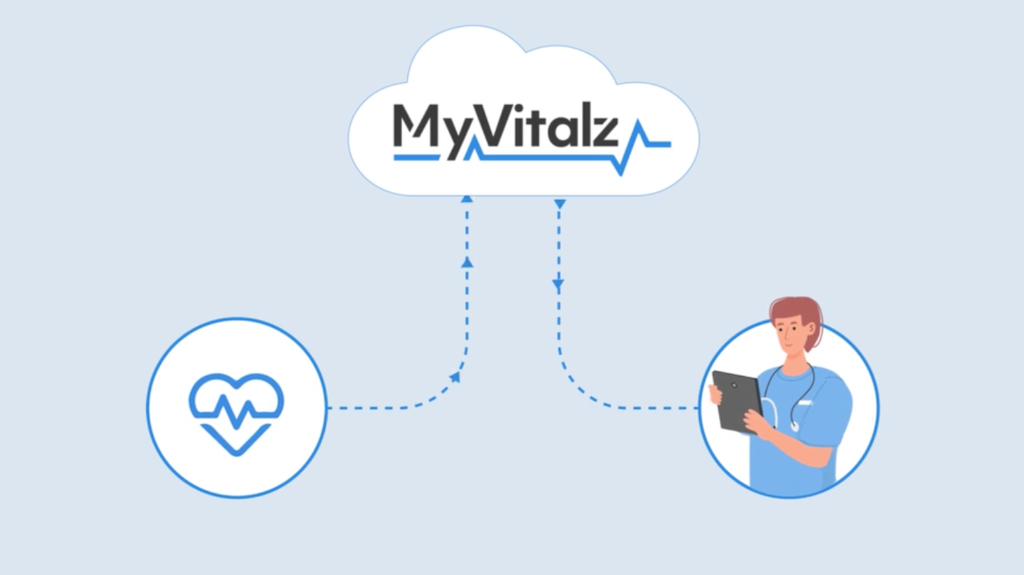
How It Works
MyVitalz is a user-friendly system designed to connect at-home patients with their in-office providers seamlessly, securely, and accurately. Our Bluetooth and Cellular technology compiles biometric health data generated by the patients’ use of in-home medical devices. These devices transmit data wirelessly to the MyVitalz cloud where the data and our advanced analytics assist the Provider team in prioritizing care and potential interventions.